Site Search:
MedicareHelp.org is a privately-owned Non-governmental agency. The government website can be found at HealthCare.gov.
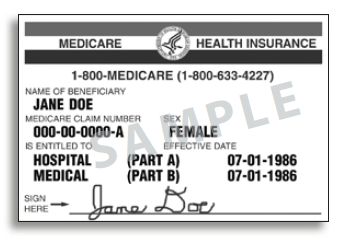
Please contact Medicare.gov, 1-800-MEDICARE, or your local State Health Insurance Program (SHIP) to get information on all of your options. Enrollment depends on the plan’s contract renewal.
Every year, Medicare evaluates plans based on a 5-star rating system.